Automate Workflow for Review Choice Demonstration
Alora’s RCD Monitor is a game-changer for Medicare certified agencies.
With Medicare’s pre-claim review requirements, home health agencies are left chasing down doctors, signatures and documentation, making process chaotic. Meanwhile, the clock ticks as claim submission, reimbursement and cash flow rely on these documents.
Alora’s Review Choice Demonstration (RCD) Monitor tracks each patient and displays a color-coded status of each related document right in the dashboard. Say goodbye to clumsy and inefficient spreadsheets. In seconds, you can see the entire documentation status for a patient.
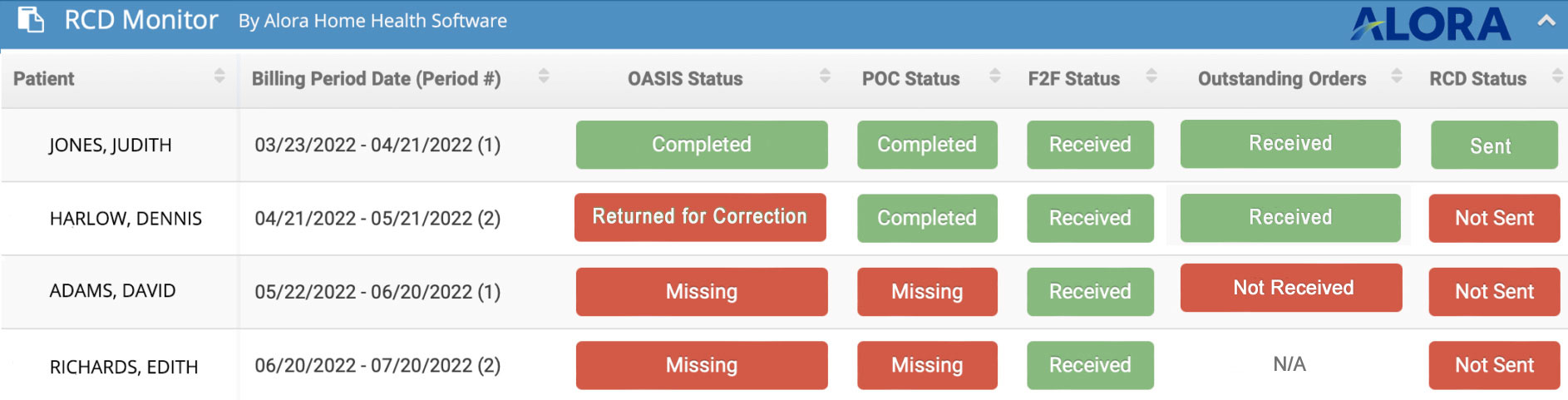
Even better, the tool allows multiple stakeholders to access the information, creating a centralized workflow and allowing you to work together as a team. You have 30 days. When your billing is on time, your cash flow is unimpeded.
With Alora’s RCD Monitor, you’ll create and continue a far more consistent routine, keeping your cash flow regular while getting paid faster.