Alora’s Prior Authorization Management functionality is designed to handle the full range of payer authorization models, from simple limits to highly complex, overlapping authorizations. It helps agencies stay compliant with payer requirements while reducing manual effort and errors.
Agencies can enter prior authorization details individually for each patient or quickly create recurring authorization entries based on predictable patterns, such as weekly or monthly visit limits that extend over longer periods.
Alora Pediatric Homecare Software also supports overlapping authorizations, ensuring the correct authorization is applied to the correct visit.
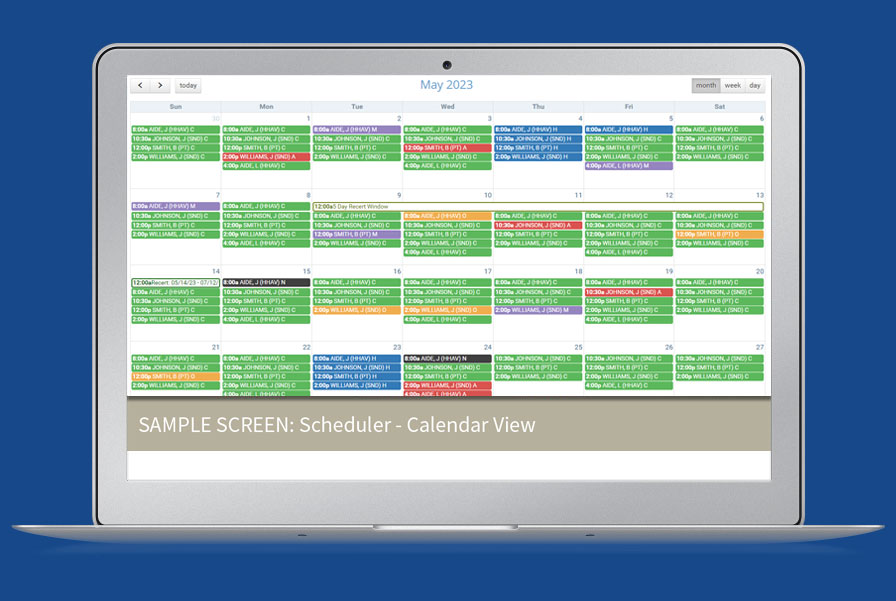
To prevent overutilization and denied claims, Alora’s scheduler actively monitors authorization usage in real time, providing automatic alerts and optional hard stops when limits are reached or no authorization is available.
Powerful reporting tools help agencies stay ahead of upcoming expirations, track authorization utilization across the organization, and proactively address issues before they impact care or revenue.
When it’s time to bill, authorization codes automatically flow into claims, streamlining the billing process and improving claim accuracy.